The Perioperative medicine team at UHS are pioneering the use of our online personal health record My Medical Record to help prepare patients for surgery.
Perioperative Medicine Lead Nurse Imogen Fecher describes how this cutting-edge approach benefits patients, staff and the Trust alike.

A patient completing our online health screening questionnaire in My Medical Record
Perioperative care and My Medical Record
Perioperative care is the care given to patients from the point of contemplation of surgery through to discharge and recovery following surgery.
The aim of perioperative care is to prepare the patient physically and mentally for surgery so that they have a reduced risk of complications from surgery and recover better.
The perioperative team has begun using My Medical Record, a secure online personal health record available to all UHS patients, to assess, communicate and exchange information with potential candidates for surgery before their operations take place.
Health screening questionnaire
The perioperative care team uses My Medical Record to collect health information on patients referred to our service.
Our health screening questionnaire within My Medical Record enables us to assess patients’ risk of complications following surgery and lets the team put a personalised plan in place, such as referral to dietitians and specialist medical teams, including cardiology and diabetes.
It also alerts the team of those patients at greatest risk of complications allowing us to arrange a 1-to-1 Shared Decision Making consultation with a consultant anaesthetist to discuss risk and potential alternatives to surgery.
This enables the patient to make an informed decision about the right treatment for them.
Once the patient has completed the online questionnaire, information and advice is also immediately provided to them on the areas they need to work on e.g. quitting smoking, reducing alcohol, increasing exercise.
This advice is given with signposting to where patient can get more information.
Once they have completed the questionnaire, the patient’s information is listed on our new Clinician Dashboard that was developed alongside the questionnaire.
The Dashboard enables the clinical teams to triage the patients in one place and document plans, which is later updated to their clinical record.
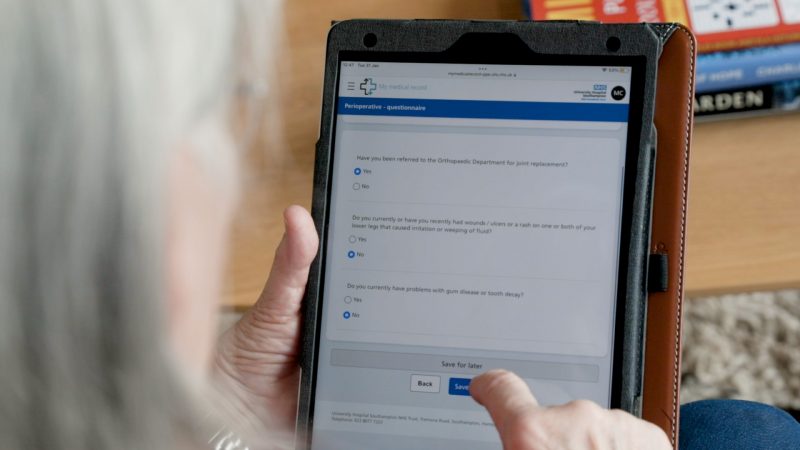
The questionnaire is simple to complete.
An innovative approach
We have incorporated My Medical Record into perioperative care because it enables us to gather information as early as possible without the need to bring patients into another outpatient appointment.
The earlier we get the information the sooner we can put together a plan of care that will improve recovery.
We previously collected this health information at the preoperative assessment appointment that occurs around one week before surgery.
This left very little time to optimise patients and often led to delays in surgery or cancellations on the day because the patient was not fit enough.
We also kept lists of patients on spreadsheets which could easily be corrupted and reliant on human input of details.
The new approach is much more secure and reliable.
Watch Imogen explain how to complete the health screening questionnaire
Early positive results
The initial engagement with the system from patients has been really encouraging.
We have already received more than 800 completed questionnaires from patients.
The majority of patients have been able to complete the questionnaire independently from home. We also have a team at the hospital who can help them to complete it if they need additional support.
The results have been early identification of those at most risk, allowing us the time to refer to specialist teams for optimisation, as well as early referral for shared decision making discussions when appropriate.
This means that patients are able to have a more personalised care plan and are given the advice and support they need to prepare for surgery.

UHS staff can support patients in completing the online form
It has been very exciting to be part of this project. We have been working on it for three years and now to see the benefits being realised is amazing.
As a trust we are very much ahead of the game nationally with our approach to screening and triage. I am proud to be part of such a forward thinking team.
Collaborating with digital colleagues
It took years to get to where we are – starting from scratch as there was no ‘off the shelf’ solution available that would do everything we needed it to.
It was also challenging trying to translate our vision into a reality.
Working closely with the digital team to help them to understand what we needed and then work with their suggestions. It was a very iterative process that still has a way to go as we will continue to refine the questionnaire based on our patient feedback.
As clinicians we had little insight into the layers of programming it takes to build these solutions and the digital team didn’t have the clinical knowledge, so we learnt from each other.
It took a long time and highlighted the need to invest time right at the start on being clear about exactly what we wanted the system to do.
It really helped having a digital lead who was also a clinician and therefore sat in both camps so to speak.

Patients can complete the questionnaire in less than 15 minutes.
Lessons learned
Working through process maps and planning into order to get the specifics down on paper before approaching the digital team was something we initially struggled with.
It was also important to be realistic about how long things would take, and to be aware that I.T. systems in the Trust were also simultaneously evolving, so that functionality we thought wasn’t possible at the start of the project was possible by the time we finished.
Having the clinical digital lead was pivotal in this project’s success.
It’s been a great experience and a steep learning curve that has a resulted in a product that really is improving practice and patient care.
